Is the U.S. getting close to being able to reopen, after weeks of social distancing? Experts say more work needs to be done ramping up systems like drive-through COVID-19 testing centers.
Matias J. Ocner/Miami Herald/Tribune News Service via Getty Images
hide caption
toggle caption
Matias J. Ocner/Miami Herald/Tribune News Service via Getty Images

Is the U.S. getting close to being able to reopen, after weeks of social distancing? Experts say more work needs to be done ramping up systems like drive-through COVID-19 testing centers.
Matias J. Ocner/Miami Herald/Tribune News Service via Getty Images
First things first: It’s not yet time to end social distancing and go back to work and church and concerts and handshakes.
Public health experts say social distancing appears to be working, and letting up these measures too soon could be disastrous. Until there is a sustained reduction in new cases — and the coronavirus’ spread is clearly slowing — we need to stay the course.
Still, society can’t stay shut down forever. Public health and state leaders are starting to talk about how and when to relax social distancing guidelines, and President Trump is expected to soon announce finalized guidelines to help states make those decisions. Even then, it’s clear that life won’t go back to normal all at once. The decisions will be staggered, and a lot of it will come down to local and regional circumstances.
“We have to do it strategically and safely,” said Dr. Monica Bharel, commissioner of the Massachusetts Department of Public Health, at a briefing by the Association of State and Territorial Health Officials Wednesday. “The worst possible outcome of reopening public life would be a second wave of this pandemic.”
Public health leaders agree that in order to safely lift social distancing restrictions we must create and sustain systems that can rapidly stamp out any new coronavirus flare-ups so they don’t spiral out of control. Here are five key things health experts say must be addressed as we begin to start businesses and community life up again.
1. Improve rapid testing
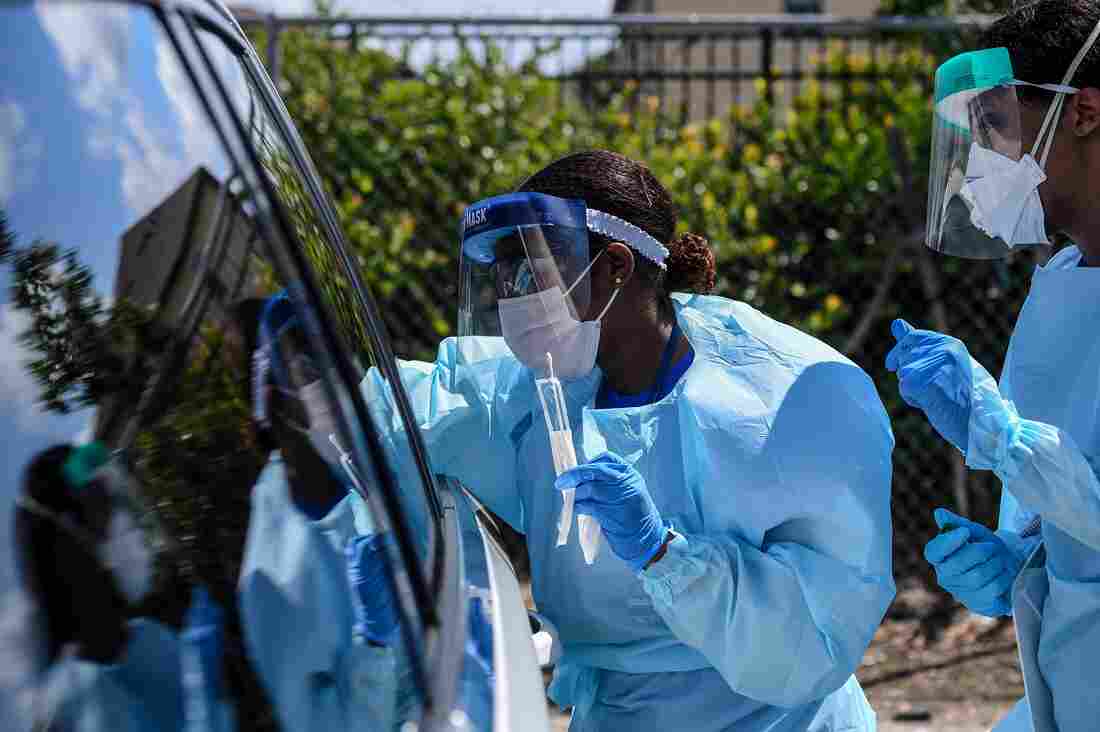
Medical personnel take patient samples at a drive-through coronavirus testing site in West Palm Beach, Florida, Monday, March 16, 2020.
Chandan Khanna/AFP via Getty Images
hide caption
toggle caption
Chandan Khanna/AFP via Getty Images
Among public health leaders, the mantra for stopping coronavirus from surging is “test, trace and isolate.” Widespread testing with fast results is the first step — if we don’t have enough tests, we don’t know where the virus is spreading. This has been a major sticking point in the U.S. response to the coronavirus, though progress has been made.
A test that provides results in less than 15 minutes is now available in some hospitals and doctor’s offices. The company that produces it, Abbott, says it is able to provide about 50,000 tests per day. It runs on the same platform that doctors use to do quick, in-office strep or flu tests.
Dr. Rachel Levine, Pennsylvania’s secretary of health, said these types of quick tests will be “really critical” to broaden access to testing, but so far her state has had trouble getting them. “We have to make sure that [there is] access in vulnerable communities,” particularly for members of Hispanic and African American communities, she said.
Nationally, there are more than 120,000 COVID-19 tests being done every day, but experts say we need to continue to ramp this up. “You want to be doing [tests] at mass scale,” says Dr. Scott Gottlieb, former head of the Food and Drug Administration, who has developed a road map to reopening at the American Enterprise Institute. He says that could mean doing several million tests every week.
One big challenge labs have had in scaling up testing has been shortages of supplies, such as swabs to collect the samples, special fluids needed to safely transport them, and reagent chemicals to extract and analyze the genetic material from the virus. Labs around the U.S. and around the world are competing for these same supplies as demand surges globally.
Reliable serological tests — also known as antibody tests — are also key to getting a handle on how much of a community’s population has already been exposed to the virus. Once someone has been exposed to the virus, their blood contains antibodies made by their immune system to fend off the infection. Serological blood tests, which can be performed quickly with a prick blood-draw, can detect these.
Several of these tests have been developed, but it’s not yet clear how reliable they are and it’s a big effort to scale up availability. “This is really a late summer, early fall kind of endeavor — these tools probably aren’t going to all be fully deployed in time to help us get out of the current epidemic,” Gottlieb says.
2. Massively upgrade contact tracing capacity
The next step in “test, trace, isolate” is “trace” — a shorthand for contact tracing. By tracking and communicating with the contacts of a confirmed COVID-19 case who are themselves at risk for infection, health workers can dramatically slow the chain of transmission.
It’s a labor-intensive process and the U.S. currently lacks the workforce to do this nationally. The head of the CDC told NPR last week that the agency is working on a big plan to scale up the workforce, though the details have yet to be released. An analysis by the Johns Hopkins Center for Health Security found the country may need 100,000 contact tracers, which would cost an estimated $3.6 billion. Dr. Tom Frieden, a former director of the Centers for Disease Control and Prevention, estimates the country may need even more, on the order of 300,000.
States are scrambling to ramp up contact tracing now. “We will need to beef up our workforce,” said Levine, the Pennsylvania health secretary. She said her state will hire more people and may use volunteers, too.
Health officials from other states agreed about the urgent need to expand contact investigations. “The capacity has been essentially overwhelmed,” says John Wiesman, the secretary of health for Washington state. “We need to redouble and triple efforts here around the pieces of case and contact investigation.”
The push to expand contract tracing quickly may go high-tech. Google and Apple are collaborating on a new system to develop apps for contact tracing, similar to those used in places like Singapore. There are privacy concerns with using smartphones to track people’s movements and contacts, and these apps are still in development, so even this shortcut will still take some time.
3. Create systems to isolate the sick and protect the vulnerable
Once the contacts of COVID-19 patients are traced, many will need to separate themselves from society for two weeks to be sure they are not infectious. There needs to be a support structure in place to make that possible, says Dr. Harvey Fineberg, a health policy researcher at the Harvard T.H. Chan School of Public Health.
“Part of a complete strategy for quarantine is that you provide places apart from the home and community where those who’ve been exposed can — in a comfortable setting — spend the time of their quarantine where they are not going to infect others,” he says.
This approach has been used in countries like China and South Korea where the coronavirus appears to be largely under control. Fineberg says it could be important for those who don’t have the space or resources to separate themselves safely from their household. “We have empty hotels all over America,” he adds.
Hotels have started to be offered as housing for health care workers concerned about infecting their family members but, Fineberg says, there is not currently a national plan to roll out quarantine centers more broadly.
Frieden, the former CDC director, agrees that places like hotels and dorm rooms may need to be part of America’s effort to get a handle on the coronavirus. “We need to think of this as an all of society response,” he says. “The countries that have had the best results, they’ve tested huge numbers of patients, and they’ve isolated patients not just in their own home, but in special facilities for people who don’t need hospitalization but don’t want to spread it to their family members.”
This kind of approach could be especially important for anyone who lives in close quarters with a lot of people — for instance, those in long-term care facilities, prisons or nursing homes.
“Ground zero for COVID-19 in this country is nursing homes,” says Frieden. “When COVID gets into a nursing home, it can really cause devastation. We need to do everything possible to stop spread in congregate facilities like nursing homes.”
Homeless shelters are a concern as well. Officials in Washington state, California and New York City have already started to use hotels and motels to house homeless residents who live in coronavirus hotspots.
4. Build up hospital capacity and the PPE supply chain

Hospitals in many places still struggle to get enough PPE and are getting creative about solving this. A nonprofit fashion design incubator in Tempe, Arizona, F.A.B.R.I.C., converted its warehouse to make isolation gowns for health care workers.
Ross D. Franklin/AP
hide caption
toggle caption
Ross D. Franklin/AP
Hospitals have been scrambling to be able to handle more and more COVID-19 patients, but there’s still work to be done to make sure they’re ready for possible new waves of infections.
“It’s a certainty that cases will increase when you relax social distancing,” says Dr. Amesh Adalja of the Johns Hopkins Center for Health Security. “It’s just: Will it be at a slow enough clip that hospital capacity will not be compromised?”
Hospitals are still struggling to source many essential supplies to allow them to serve a surge of patients. There’s regional variation, but the AEI road map suggests that, on average, hospitals need to double their intensive care unit and ventilator capacity to care for critically ill COVID-19 patients, and that the supply of personal protective equipment should be stable so health care workers can protect themselves from infection.
Adalja is encouraged by efforts by hospitals and communities to share resources with each other, so that limited equipment can be targeted to the right places. He said that progress has already been made in “being able to rapidly move ventilators from one part of a country to another part of the country as the need arises.” A public-private partnership called the “Dynamic Ventilator Reserve,” announced on Tuesday, aims to facilitate this kind of coordination between hospitals across the country.
5. Zero in on effective treatments
At the moment there’s no clear evidence on an effective therapy for COVID-19. Right now, it’s a waiting game as data on various treatments start to roll in.
The Milken Institute is tracking dozens of different clinical trials underway to test treatments. Researchers are testing everything from antibody-based therapies to antiviral medicines, as well as existing drugs including hydroxychloroquine that could be repurposed to help treat COVID-19. It’s too soon to say if drugs such as the antiviral remdesivir, are effective, but the company behind this drug says it will have some preliminary results from a study at the end of April.

After weeks of social distancing, streets in Washington, D.C., and many other towns and cities are often empty. The pressure is growing to get society moving again.
Eric Baradat/AFP via Getty Images
hide caption
toggle caption
Eric Baradat/AFP via Getty Images
“Maybe in weeks or months, we may start to get some data from some of the experimental drugs to see how well they work,” says Adalja. “But truly, unequivocally effective antiviral treatment may take some time to develop.” A simple pill to treat coronavirus outside of a hospital, like Tamiflu for influenza, is even further out, he says.
Gottlieb says the combination of effective treatments as well as expanded testing and surveillance would put us in a situation where we can live with the virus, instead of being paralyzed by it.
“I think that [would be] a robust enough set of tools that this could become a livable threat, that we can get back to a fairly normal way of life and be able to mitigate the risk from coronavirus even before we have a vaccine in place,” he says. “Now, life will never be perfectly the same until we have a vaccine that can fully vanquish it.”
There are dozens of compounds being evaluated for the development of a vaccine, but that’s at least a year off.
Rob Stein and Nurith Aizenman contributed reporting